What is it?
The Pre-authorization and Referral submission workflow is part of the membership view. Provider offices would see a patient and then submit an authorization or referral to the health plan using our tool. During one-on-one research sessions, while mapping out their workflow, I discovered the challenges office staff faced in entering the required data into our system.
Understanding its impact
Once I had a suspicion that there was a problem, the next step was to ascertain the extent of its impact. To do this, I reached out to our external health plan partners and arranged meetings to review their reports with them and gain a deeper understanding of their workflow through observation. This is where I confirmed that addressing issues in our pre-authorization and referral submission workflows would have a substantial impact on users' time.
We spend a about 50% of our time fixing authorizations rather then approving or denying them. I spend a lot of time on the phone with providers trying to help them submit correctly.
So the health plans just kind of accepted that this was part of their workflow. Let's fix it!

Next Steps
To gain a deeper understanding of the problem, I consulted knowledgeable individuals from organizations that partner with us but do not necessarily use our toolset. These experts, who are well-versed in the typical pre-authorization workflow, underwent testing with our current offering to help identify pain points.
This list is ridiculous, which one is the right one? I’ll just pick this one and write what I want in the comments.
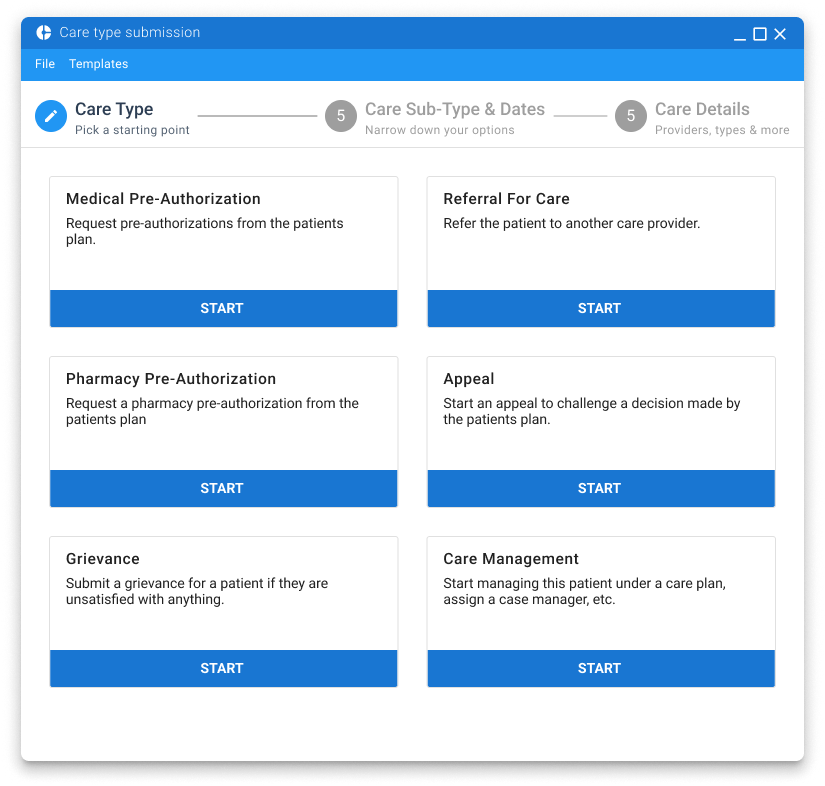
Houston, we have identified problems. The extensive list of authorizations and referrals made it difficult to discern what was required. Additionally, all the options were intermixed, providing no clarity on their respective placements.
I believe that...
Based on these research sessions, I believe that segmenting pre-authorizations and referrals into separate types will reduce errors within the provider submission flow.
Goal
Reduce Errors on submission - requiring less intervention at the plan level.
Putting in the work
To test if segmenting pre-authorizations and referrals into separate types was the correct assumption, I scheduled a card sorting session with the previously mentioned health plan partners and provider office staff. In these sessions, we organized groups into primary care types and sub-care types.
The next steps were to create a workflow to take advantage of this segmentation. By segmenting into Care Types, we could effectively control what data was presented specifically to the type of care they were submitting. Naturally, this led us into a wizard-like stepper flow concept.
Let's make it
Based on feedback and prototype usability testing, we decided we had gained sufficient knowledge to initiate development. During the development process, constant refinements were made to our testable Sketch/InVision prototype..
Results
Based on workflow reports, we reduced the time spent by health plan staff on fixing submissions and coaching providers by 90%. Feedback has been positive across all workflows. However, we continue to improve this workflow and recently introduced templates, which save provider submission time, increase happiness, and reduce effort measurably.
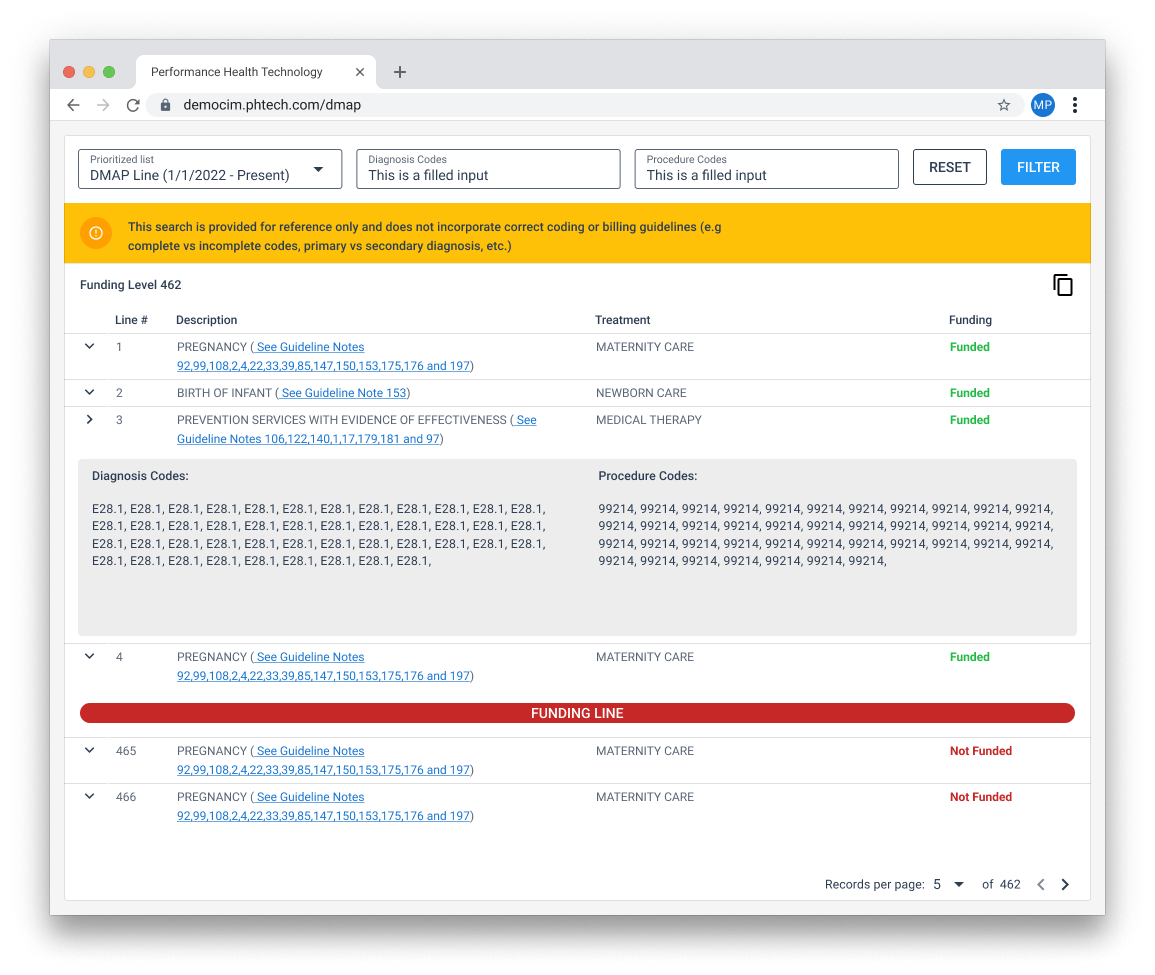
We also took the time to offer a toolset that allows providers to look up ICD-10 codes and determine if they are billable. (This is worthy of a separate write-up.)